Massage therapy is often associated with spas and relaxation, but Clinical Massage Therapy represents a far more targeted and impactful approach. Rooted in anatomical and physiological knowledge, clinical massage has evolved into a respected discipline that plays an increasingly significant role in integrative and mainstream healthcare. From managing chronic pain to improving post-surgical recovery, its applications are broad, scientifically grounded, and highly effective.
Massage therapy is often associated with spas and relaxation, but Clinical Massage Therapy represents a far more targeted and impactful approach. Rooted in anatomical and physiological knowledge, clinical massage has evolved into a respected discipline that plays an increasingly significant role in integrative and mainstream healthcare. From managing chronic pain to improving post-surgical recovery, its applications are broad, scientifically grounded, and highly effective.
– What Is Clinical Massage Therapy?
Clinical Massage Therapy is a treatment-oriented modality that focuses on addressing specific musculoskeletal issues. Unlike general relaxation massage, it is:
- Goal-directed, often prescribed or recommended by physicians or physical therapists.
- Evidence-informed, relying on assessment, documentation, and measurable outcomes.
- Therapeutically focused, using advanced techniques like myofascial release, trigger point therapy, and neuromuscular therapy.
Practitioners typically work in clinical settings such as hospitals, chiropractic clinics, rehabilitation centers, or private practices specializing in pain management.
The Role of Clinical Massage in Healthcare
- Pain Management
Perhaps the most recognized contribution of clinical massage is its role in managing acute and chronic pain. It is commonly used for conditions like:
- Lower back pain
- Sciatica
- Neck and shoulder pain
- Migraines
- Temporomandibular joint dysfunction (TMJ)
Massage techniques help increase blood flow, reduce muscle tension, and stimulate endorphin release, offering both immediate relief and long-term improvement.
- Injury Rehabilitation
After an injury—be it from sports, accidents, or repetitive strain—massage therapy facilitates faster healing by:
- Breaking down scar tissue
- Improving circulation
- Enhancing lymphatic drainage
- Restoring range of motion
Clinical massage therapists often collaborate with physical therapists to create tailored recovery plans.
- Post-Surgical Recovery
Surgical procedures often leave patients with inflammation, adhesions, and restricted mobility. Clinical massage can:
- Reduce post-operative swelling
- Improve circulation to surgical sites
- Ease pain without the need for high doses of medication
- Accelerate the return to physical function
- Support for Chronic Conditions
Massage is increasingly used as part of the care plan for individuals with chronic illnesses such as:
- Fibromyalgia
- Arthritis
- Multiple sclerosis
- Cancer-related pain and fatigue
These conditions often resist conventional treatments or come with undesirable side effects. Massage provides a non-pharmacologic, patient-centered solution that enhances comfort and quality of life.
– Clinical Massage in Integrative and Preventive Care
The healthcare industry is shifting toward preventive, integrative, and patient-centered models. Clinical massage is aligned with this shift, offering:
- Proactive stress reduction, which helps prevent stress-related illness.
- Improved sleep quality, supporting overall health.
- Immune system support, through improved lymphatic circulation.
- Muscle balance and posture correction, preventing future injuries.
Increasingly, clinical massage therapists are part of integrative health teams working alongside doctors, nurses, chiropractors, psychologists, and other professionals to provide holistic care.
– Scientific Support and Growing Recognition
A growing body of research supports the efficacy of clinical massage. For example:
- A 2016 meta-analysis in Pain Medicine found that massage significantly reduces pain intensity in conditions like fibromyalgia and lower back pain.
- The American College of Physicians now includes massage therapy in its guidelines for the treatment of back pain.
- Healthcare providers like the Veterans Health Administration (VHA) and Kaiser Permanente have integrated massage therapy into their pain management programs.
This recognition is fostering greater insurance coverage, more formalized training programs, and increased collaboration between massage therapists and other health professionals.
– Training and Professional Standards
Clinical massage therapists require specialized training beyond basic certification. Programs typically include:
- Advanced anatomy and kinesiology
- Pathology and clinical assessment
- Orthopedic and neuromuscular techniques
- Documentation, ethics, and inter-professional communication
Graduates often pursue credentials like the Board Certification in Therapeutic Massage and Bodywork (BCTMB) or specialize in areas like oncology massage or sports therapy.
– The Future of Clinical Massage Therapy
The future is bright for clinical massage therapy as:
- Public demand grows for non-invasive, drug-free treatment options.
- Insurance and regulatory frameworks increasingly support integrative therapies.
- Technology enhances documentation and outcome tracking, further validating massage’s role in evidence-based care.
As healthcare continues to prioritize holistic, cost-effective, and personalized treatment, clinical massage will remain a vital component of patient well-being and recovery.
– Conclusion
Clinical Massage Therapy is far more than a luxury—it’s a critical therapeutic intervention that bridges the gap between physical therapy and traditional medicine. With proven benefits, growing scientific validation, and a focus on individualized care, clinical massage continues to carve out its rightful place within modern healthcare systems. Whether you’re a patient, provider, or prospective student, understanding the role of massage in clinical care can unlock new pathways to health, healing, and holistic wellness.







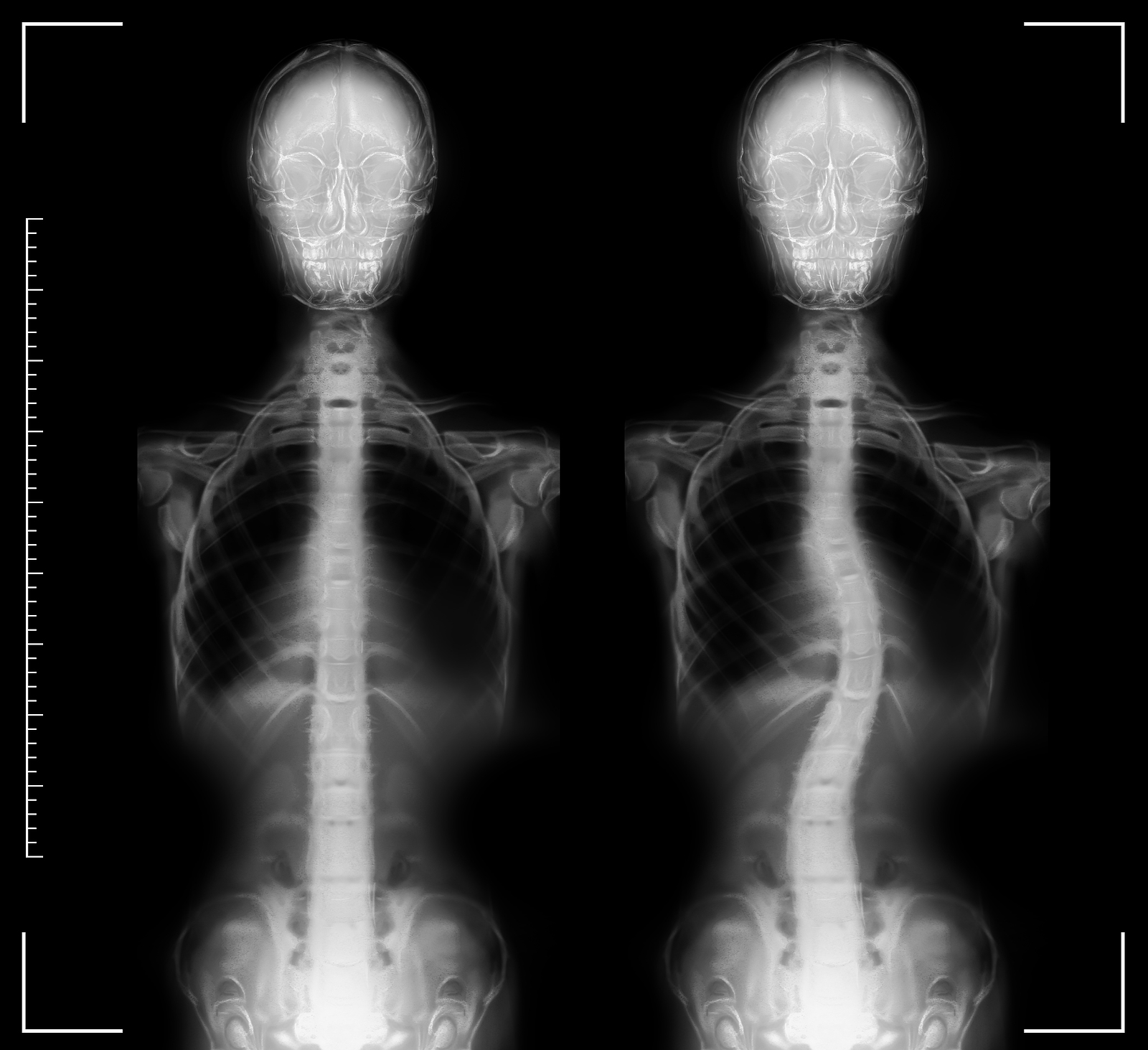 Introduction: Scoliosis is a complex spinal condition characterized by an abnormal curvature of the spine, often resulting in pain, discomfort, and limited mobility. While traditional treatments like bracing,
Introduction: Scoliosis is a complex spinal condition characterized by an abnormal curvature of the spine, often resulting in pain, discomfort, and limited mobility. While traditional treatments like bracing, 
 Massage therapy is a holistic healing modality that has gained widespread recognition for its ability to promote relaxation, reduce stress, and address musculoskeletal issues. While massage therapists are primarily trained in techniques that target muscles and soft tissues, it is crucial for them to have a comprehensive understanding of their clients’ neurological health. Incorporating thorough neurological assessments into massage therapy sessions allows therapists to gather vital information about the nervous system’s function, which can greatly enhance the effectiveness and safety of the treatment. In this extensive blog post, we will delve into the importance of neurological assessments in massage therapy and how they contribute to the overall well-being of clients.
Massage therapy is a holistic healing modality that has gained widespread recognition for its ability to promote relaxation, reduce stress, and address musculoskeletal issues. While massage therapists are primarily trained in techniques that target muscles and soft tissues, it is crucial for them to have a comprehensive understanding of their clients’ neurological health. Incorporating thorough neurological assessments into massage therapy sessions allows therapists to gather vital information about the nervous system’s function, which can greatly enhance the effectiveness and safety of the treatment. In this extensive blog post, we will delve into the importance of neurological assessments in massage therapy and how they contribute to the overall well-being of clients.
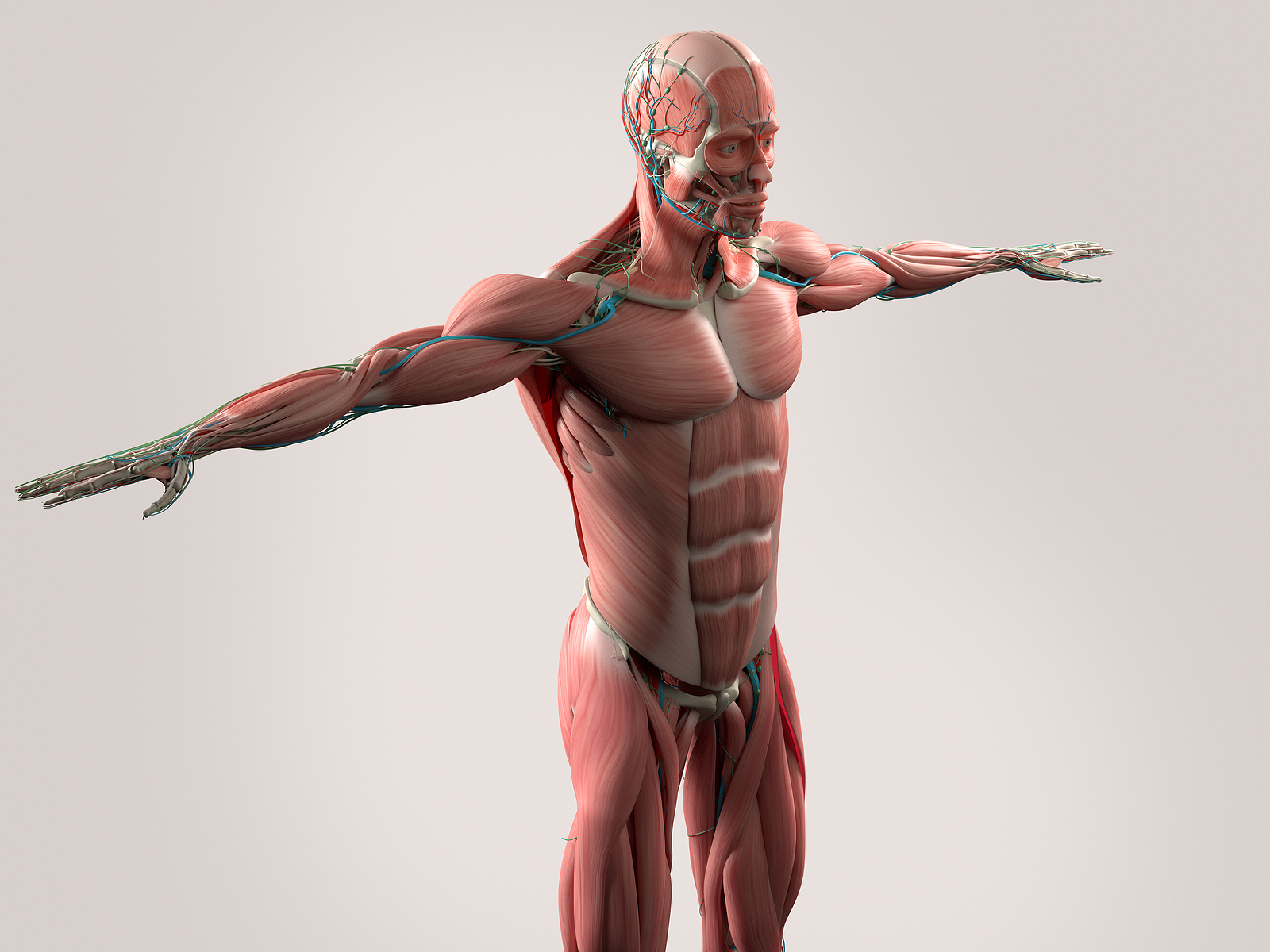 Introduction: In the realm of holistic healthcare, the human body continues to reveal hidden complexities, and one such marvel is the connective tissue known as fascia. Long overlooked and undervalued, fascia has gained significant attention in recent years due to its profound impact on our overall well-being. Fascia serves as a matrix that holds our body together, providing structural integrity and facilitating communication between different parts of our system. In this blog post, we delve into the importance of fascia and explore how massage therapy directly affects this remarkable tissue.
Introduction: In the realm of holistic healthcare, the human body continues to reveal hidden complexities, and one such marvel is the connective tissue known as fascia. Long overlooked and undervalued, fascia has gained significant attention in recent years due to its profound impact on our overall well-being. Fascia serves as a matrix that holds our body together, providing structural integrity and facilitating communication between different parts of our system. In this blog post, we delve into the importance of fascia and explore how massage therapy directly affects this remarkable tissue.
 As a complementary and
As a complementary and