
Thermotherapy and Endurance Athletics: How Heat Can Boost Performance and Speed Recovery
Endurance athletes like marathon runners and Ironman competitors push their bodies to the limit. From the mental stamina required to stay focused for hours to the physical stress placed on muscles, joints, and connective tissues, it’s no wonder that recovery and performance optimization are top priorities. Among the tools used by athletes and trainers alike, thermotherapy—the use of heat for therapeutic purposes—has gained popularity for its ability to enhance preparation before exercise and support recovery afterward.
In this article, we’ll explore the science and practical benefits of thermotherapy for endurance athletes, with a deep dive into how it can be used before and after intense exercise like marathons or Ironman competitions.
What is Thermotherapy?
Thermotherapy refers to the application of heat to the body for therapeutic benefits. It can be delivered through various methods including:
-
Moist heat (hot towels, steam rooms)
-
Dry heat (heating pads, infrared saunas)
-
Hydrotherapy (hot baths, whirlpools)
-
Paraffin wax treatments
-
Contrast therapy (alternating hot and cold treatments)
While many people associate heat therapy with relaxation, its physiological effects go far beyond comfort.
Pre-Event Thermotherapy: Warming Up More Than Just Muscles
1. Increased Blood Flow and Oxygen Delivery
Before any strenuous activity, muscle elasticity and blood circulation are key. Applying heat pre-exercise helps:
-
Dilate blood vessels
-
Boost circulation to the muscles
-
Increase the oxygen and nutrient delivery needed for sustained effort
This can lead to enhanced flexibility and reduced muscle stiffness, which helps prevent strains or injuries during the race.
2. Neuromuscular Activation
Heat stimulates nerve endings and can increase neuromuscular responsiveness. For endurance athletes, this can translate into improved coordination, balance, and proprioception, especially important for triathlon segments like cycling and running.
3. Mental Preparation and Relaxation
Applying heat pre-race can also support mental focus. Whether it’s a sauna session or warm compress, heat triggers the parasympathetic nervous system, promoting a calm, centered mindset before the adrenaline rush of competition.
Pro Tip: Try a short sauna session (10–15 minutes) or warm bath 2–3 hours before your race. Pair it with light dynamic stretching to prime your body for peak performance.
Post-Event Thermotherapy: Enhancing Recovery and Repair
After crossing the finish line, the real work begins—recovery. Endurance events cause microtears in muscle fibers, inflammation, and lactic acid buildup. Thermotherapy can be a powerful tool in this phase.
1. Muscle Relaxation and Pain Relief
Heat promotes muscle relaxation by decreasing muscle spindle sensitivity, reducing spasms, and calming soreness. This is especially beneficial for areas like the hamstrings, calves, and quads, which bear the brunt of long-distance events.
2. Improved Metabolic Waste Removal
By increasing circulation post-event, heat helps flush metabolic byproducts like lactic acid and cytokines from tissues. This accelerates the healing process and reduces delayed onset muscle soreness (DOMS).
3. Tissue Healing and Joint Support
Heat can increase the extensibility of connective tissues and may help reduce stiffness in joints, particularly in the knees, hips, and ankles. This makes thermotherapy ideal for athletes managing overuse injuries or recovering from intense training cycles.
4. Hormonal and Immune Support
Studies show that heat therapy, particularly sauna use, can increase levels of growth hormone, endorphins, and heat shock proteins, which aid in muscle repair and immune function. This is critical for endurance athletes whose immune systems can be temporarily suppressed post-competition.
Pro Tip: Apply moist heat or use an infrared sauna for 20–30 minutes 6–24 hours after the event for optimal recovery. Always ensure you’re rehydrated before and after.
Thermotherapy vs. Cryotherapy: Should You Use Heat or Ice?
Both thermotherapy and cryotherapy have their place in an athlete’s recovery toolkit. A general guideline:
-
Use heat for chronic soreness, muscle relaxation, and systemic recovery.
-
Use cold for acute inflammation, swelling, or sharp pain.
In fact, many athletes benefit from contrast therapy, alternating hot and cold treatments to stimulate circulation and reduce inflammation while promoting healing.
Precautions and Best Practices
While thermotherapy is safe for most people, it’s important to use it correctly:
-
Avoid heat immediately after acute injury, where inflammation and swelling are present.
-
Limit sauna or hot tub time to prevent dehydration or overheating.
-
Ensure proper hydration before and after any heat treatment.
-
People with cardiovascular conditions or skin sensitivities should consult a healthcare professional first.
Final Thoughts: Turning Up the Heat for Better Performance and Recovery
Thermotherapy is not just a feel-good practice—it’s a science-backed strategy that can boost performance, enhance flexibility, prevent injury, and accelerate recovery for endurance athletes.
Incorporating pre-race heat treatments like saunas or warm compresses can prime the muscles and mind, while post-event thermotherapy can minimize soreness, reduce recovery time, and help athletes bounce back stronger.
As always, listen to your body, experiment with different methods, and consider incorporating heat as part of a comprehensive training and recovery routine alongside nutrition, hydration, and sleep.
Whether you’re chasing a personal best at your next marathon or pushing the limits in an Ironman triathlon, a little heat might be the secret weapon to elevate your performance and keep you moving pain-free.
Have you tried thermotherapy in your race-day routine? Share your experiences or tips in the comments below!
To learn more about this and other topics relating to sports massage visit our website at seattlemassageschool.com







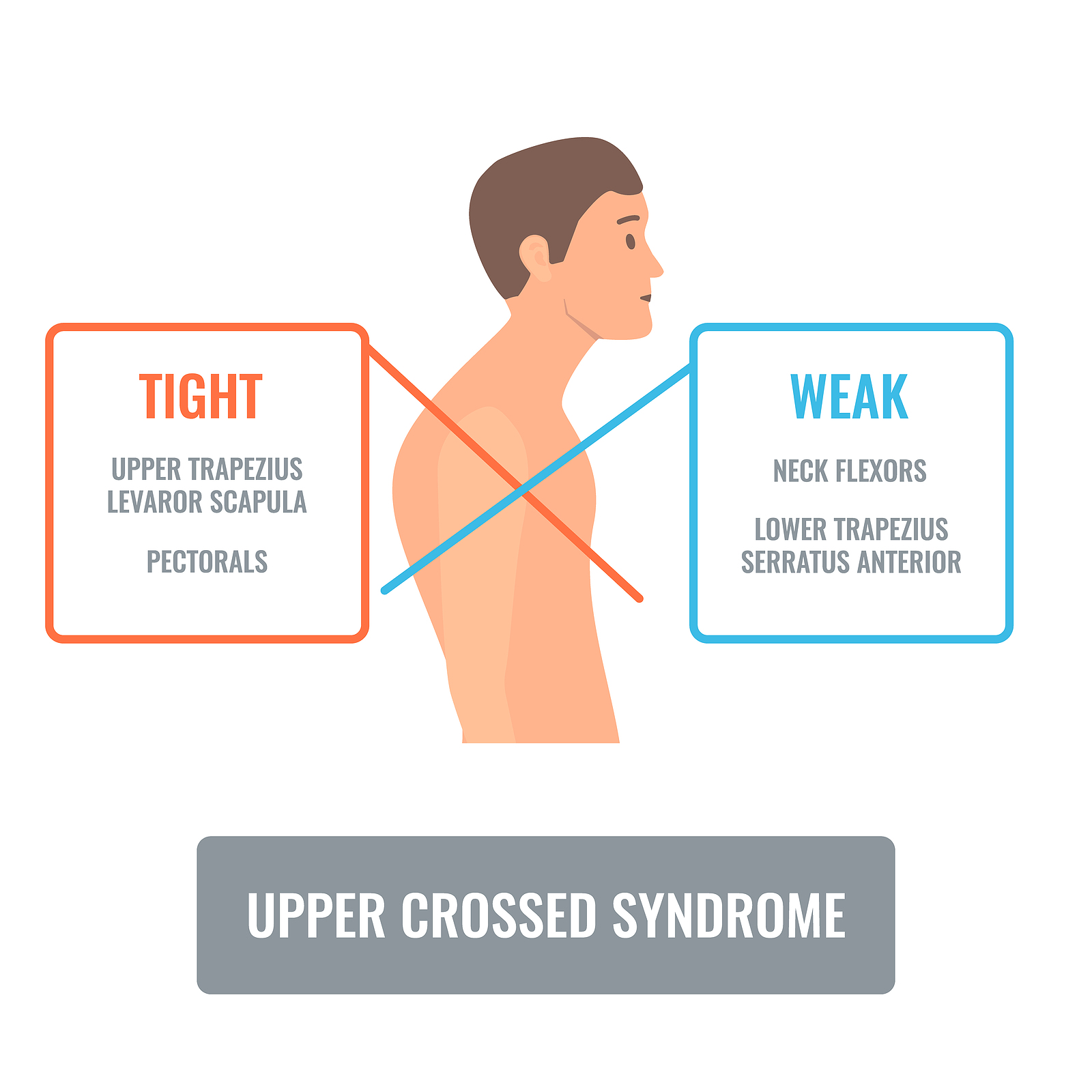 Upper Crossed Syndrome (UCS) is a muscular imbalance pattern that commonly affects individuals who have a sedentary lifestyle or spend long hours at a desk or computer. This condition results from overuse of some muscles and underuse of others, leading to a complex chain of events that can cause pain, stiffness, and discomfort in the neck, shoulders, and upper back.
Upper Crossed Syndrome (UCS) is a muscular imbalance pattern that commonly affects individuals who have a sedentary lifestyle or spend long hours at a desk or computer. This condition results from overuse of some muscles and underuse of others, leading to a complex chain of events that can cause pain, stiffness, and discomfort in the neck, shoulders, and upper back.
 As a complementary and
As a complementary and 
 Cupping therapy is an ancient form of alternative medicine that has been used for centuries to treat various conditions. It involves placing cups on the skin to create a vacuum effect that draws the skin and underlying tissues up into the cup. Cupping has gained popularity in recent years, especially among athletes, as a way to treat sports injuries and improve performance. In this blog post, we will explore cupping therapy for sports injuries and how it can benefit athletes.
Cupping therapy is an ancient form of alternative medicine that has been used for centuries to treat various conditions. It involves placing cups on the skin to create a vacuum effect that draws the skin and underlying tissues up into the cup. Cupping has gained popularity in recent years, especially among athletes, as a way to treat sports injuries and improve performance. In this blog post, we will explore cupping therapy for sports injuries and how it can benefit athletes.


